Can the Pfannenstiel skin incision length be adjusted according to the fetal head during elective cesarean delivery?
- 1Department of Obstetrics and Gynecology, Basaksehir Cam and Sakura State Hospital, Istanbul, Türkiye
- 2Department of Obstetrics and Gynecology, Cyprus International University School of Medicine, Lefkosa-TRNC, Mersin, Türkiye
- 3Department of Obstetrics and Gynecology, Cerrahpasa University School of Medicine Hospital, Istanbul, Türkiye
Objective: The study aims to determine whether the Pfannenstiel skin incision can be adjusted according to the fetal head's occipitofrontal diameter (OFD) during primary cesarean delivery.
Background: Eligible 114 nulliparous women delivered at term by cesarean section in which Pfannenstiel skin incision was performed according to the OFD of the fetal head between June 2017 and September 2021 were included. Excluded cases were non-vertex presentations, all emergency cesarean sections, severe preeclampsia, women in an active phase of the first stage of labor and second stage of labor, placenta previa and low-lying placenta, multiple pregnancies, and uncontrolled gestational diabetes mellitus.
Results: Among 114 eligible nulliparous women, the mean OFD was 116.1 ± 7.2 (99–138) mm, and the measurement of the Pfannenstiel skin incision length, which was performed according to the OFD was found to be 122.8 ± 9.2 (100–155) mm. The difference between OFD and Pfannenstiel incision kept remained within 10 mm in 90 (82.5.2%), 10–20 mm in 17 (15.5%), and more than 20 mm in two women (1.8%). This technique was successful in 109 (95.6%) out of 114 women without extending the skin incision. In five women, skin incision needed to be extended up to 38 mm. In 10 women (8.7%), the rectus abdominis muscle was cut partially to deliver the fetal head. The mean fetal umbilical artery pH was 7.33 ± 0.05. No neonatal hypoxia was encountered in the study.
Conclusion: Pfannenstiel skin incision can be adjusted according to the OFD with minimal margins of error. This technique may provide better cosmetic results by avoiding unnecessarily prolonged incisions with similar newborn outcomes.
Clinical Trial Registration: Clinicaltrials.gov, identifier [NCT05632796].
Introduction
Cesarean birth is the extraction of a baby by cutting off the abdominal wall layers to the uterus, dating back to ancient BC. Cesarean surgical techniques only evolved a little since the foremost surgical procedures were introduced as uterine lower segment transverse incision (1, 2), namely, Kerr incision (3), and the lower abdominal transverse skin incision, namely, Pfannenstiel incision (4). Pfannenstiel incision is the most frequent abdominal incision used for cesarean delivery (CD) because of its cosmetic advantages due to the level of incision (bikini cut) and the use of Langer's lines (5). Surprisingly, Pfannenstiel incision’s length has been out of interest since its introduction in 1900. Its length should be enough for the surgeon to feel comfortable and provide enough exposure during the operation (6). In the past, although a 15 cm Pfannenstiel incision length was claimed to be enough (7, 8), the given Pfannenstiel incision length ranged widely between 11.7 and 16.9 cm (7, 9–13). More than 20 cm Pfannenstiel incision length has also been reported (14).
Nevertheless, some obstetricians tend to make the incision as short as possible in the contemporary world, considering the patient's esthetic expectations. Shorter incisions may not have cosmetic advantages only; pain, wound infection, and nerve entrapment may also be less (10–12, 15–17). In addition, abdominal laparotomy incisions should be kept as small as possible to reduce surgical stress (18). To date, the length of the Pfannenstiel incision remains to be determined.
This study aims to describe a modified Pfannenstiel skin incision technique that was adjusted according to the fetal head's occipitofrontal diameter (OFD) and evaluate its short-term maternal and neonatal outcomes.
Materials and methods
Nulliparous women who underwent primary CD in which the Pfannenstiel incisions were performed according to the occipitofrontal diameter between June 2017 and September 2021 at Yakın Dogu University Hospital were evaluated. This interventional pilot study was approved by the Institution's Local Ethics Committee (30.09.2021, Number: YDU 2021/95-1398) and was registered to clinicaltrials.gov on 01/12/2022 with the registry number (NCT05632796).
The information regarding the procedure was given, and informed consent was obtained from all women.
The women older than 18 years with term nulliparous pregnancies (>37 weeks) who underwent primary CD with vertex presentation under spinal anesthesia were included.
During the evaluation of medical records, all emergency cesarean sections, including women with non-reassuring fetal heart rates and fetal distress, third trimester bleeding including abruption of placenta and placenta previa bleeding, arrest of labor in the second phase, and severe preeclampsia, were excluded. In addition, women who underwent CD with non-vertex presentations such as breech and shoulder presentation, deflexion fetal head presentations such as face and brow, those who were in the active phase of the first stage of labor, who had placenta previa and low-lying placenta, multiple pregnancies, and uncontrolled gestational diabetes mellitus were also excluded.
Primary outcomes were the final incision length following the Pfannenstiel incision skin closure, the need to extend the skin incision by the surgeon, and the difference between the initial length of the Pfannenstiel incision, which was made according to the fetal OFD and the final one. Secondary outcomes were surgical features, including duration of operation, intraoperative difficulties or additional surgical interventions during delivery of the baby, neonatal outcomes, and postoperative maternal outcomes, including wound complications.
Surgical technique
Adjusting the Pfannenstiel skin incision according to the fetal OFD technique was invented and first performed by the first author (BK); it was introduced to authors OO and AO. In this study, the three surgeons performed cesarean deliveries (BK, OO, and AO).
All women underwent ultrasound measurement of OFD and other fetal biometric measurements, including biparietal diameter (BPD), head circumflex (HC), and estimated fetal weight (EFW), just before the operation. According to the weight of pregnant women, 1–3 g of first-generation cephalosporin was given within 1 h of the skin incision. All women were subjected to regional spinal anesthesia. The abdominal skin was cleaned with a povidone-iodine solution, and the operative field was covered with sterile surgical drapes. Initially, the skin 2–3 cm above the pubic bone, where the Pfannenstiel incision will be made, was marked with the sterile skin marker pen according to the OFD measurement. The line was measured with a flexible ruler (Medbar® skin marker kit, Izmir, Türkiye). A slightly cephalad curved Pfannenstiel incision was made according to the OFD, marked on the skin (Pfannenstiel incision with Kaya modification). The fascia incision was made several centimeters more expansive than the marked skin incision (not measured). Following direct entry to the abdominal cavity with the right index finger, care was taken not to stretch the skin to avoid extending the skin incision length. The uterine lower segment Kerr incision was performed with a scalpel and opened enough with two thumbs of the surgeon to allow fetal head delivery. Fundal pressure with appropriate strength was applied to deliver the baby. Following the baby's delivery, the umbilical cord was cut, and an arterial umbilical cord blood sample was taken and sent for umbilical artery pH measurement. The pediatricians evaluated the 1- and 5-min Apgar scores in the operation room. Placentas were delivered either by the extra-abdominal placental delivery method (19) or spontaneous intraabdominal delivery up to the surgeon's preference. Uterine incision was double-layer sutured with 1 polyglactin 910 suture (Vicryl®, Ethicon, Somerville, NJ, USA). Intravenous infusion of 20 IU oxytocin in 500 ml of normal saline at a rate of 125 ml/h was started during the cesarean section and continued for 4 h after delivery. Peritoneum and fascia were closed with 2-0 and 1 polyglactin 910 suture (Vicryl®, Ethicon, Somerville, NJ, USA), respectively. The skin incision was sutured with continuous 3-0 rapid polyglactin 910 suture (Vicryl®, Ethicon, NJ, USA) and measured with a flexible ruler (Medbar® skin marker kit, Izmir, Turkey) in centimeters following completing the skin incision closure (Figure 1) (see Supplementary Videos S1, S2). The duration of the operation was accepted as the time between the incision and the skin closure. The time interval between the uterine incision and the baby's delivery was also recorded. The wounds were kept dressed until 24 h and Transparent Film spray was applied (Opsite® spray, Smith & Nephew, Belgium) following cleaning with iodine solution and then left open. Wounds were checked 1 and 6 weeks after cesarean delivery.

Figure 1. Adjusting the Pfannenstiel skin incision according to the ultrasound measurement of occiputofrontal diameter (OFD). (Pfannenstiel incision with Kaya modification). OFD's were measured as 117, 119 and 128 mm from top to bottom, respectively. Pfannenstiel incisions after closure of the skin were measured as 128, 117 and 125 mm from top to bottom, respectively.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) software version 22.0 (SPSS Inc., Chicago, IL, USA) was used for establishing the database and statistical calculations. The Kolmogorov–Smirnov test was used to evaluate the homogeneity of the distribution of continuous variables. Homogenous continuous variables were given as mean ± standard deviation (SD), calculated with one-sample t-test in all cases, and compared in subgroups with independent samples t-test. Heterogenous continuous variables were given as median (minimum–maximum), calculated with the one-sample Kolmogorov–Smirnov test in all cases, and compared in subgroups with the Mann–Whitney U-test. The categorical variables were given as n/N (%) calculated with descriptive analysis. Pearson correlation analysis was performed for the parameters affecting the Pfannenstiel incision–OFD difference. A p-value of <0.05 was accepted as statistically significant.
Results
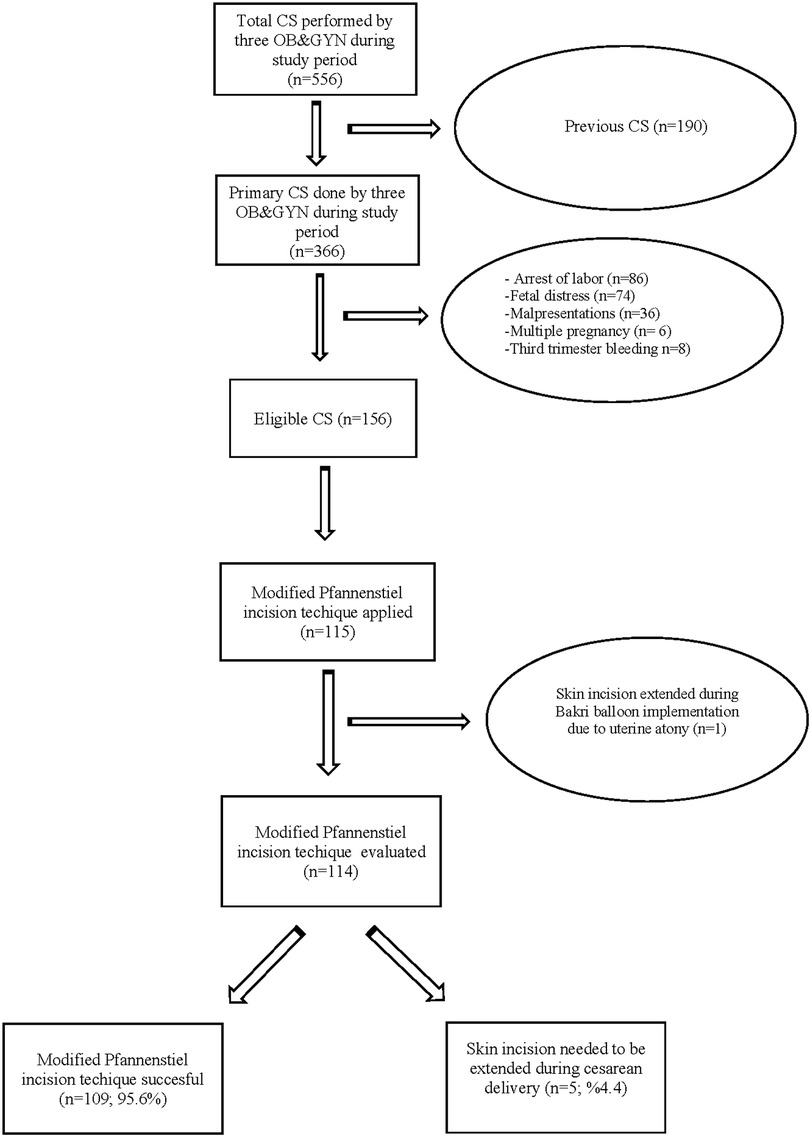
During the study period, a total of 556 cesarean deliveries were performed by the three surgeons (BK, AO, and OO). About 190 previous cesarean deliveries were excluded, and 336 women underwent primary cesarean delivery. Among the 336 primary cesarean deliveries, 210 women were excluded due to arrest of labor, fetal distress, malpresentation, multiple pregnancies, and third trimester bleeding. Finally, 115 cesarean deliveries were performed with the modified Pfannenstiel skin incision out of 156 eligible primary cesarean deliveries. In one patient, the skin incision needed to be extended following the delivery of the baby due to Bakri balloon implementation for uterine atony.
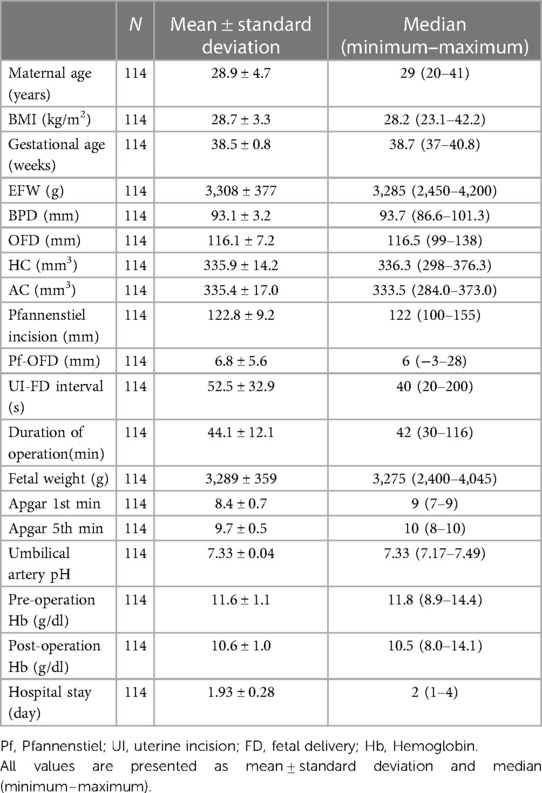
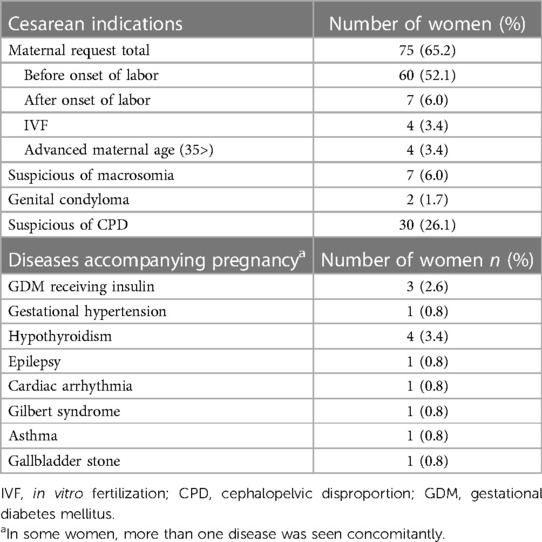
This technique was completed in 109/114 (95.6%) women without extending the skin incision (Figure 2). In five women (4.4%), Pfannenstiel skin incision needed to be extended during cesarean delivery, which was accepted as a technique failure (Table 1). Demographic characteristics of women, fetal ultrasonographic measurements, operation features, preoperative and postoperative hemoglobin levels, and neonatal outcomes of the study population are given in Table 2. The indications of CD and diseases accompanying pregnancy are given in Table 3. The Pfannenstiel skin incision, made according to the fetal OFD, was approximately 116.1 ± 7.2 mm (99–138 mm), and the final measured Pfannenstiel skin incision length after closing the skin was found to be 122.8 ± 9.2 mm (100–155 mm). The mean difference between the final and initial incisions was 6.8 ± 5.6 mm.
Figure 3 shows the relationship between the OFD and Pfannenstiel incision range. The difference between the OFD and the final Pfannenstiel incision kept remained within 10 mm in 90 (82.5%), 10–20 mm in 17 (15.5%), and more than 20 mm in two women (1.8%).
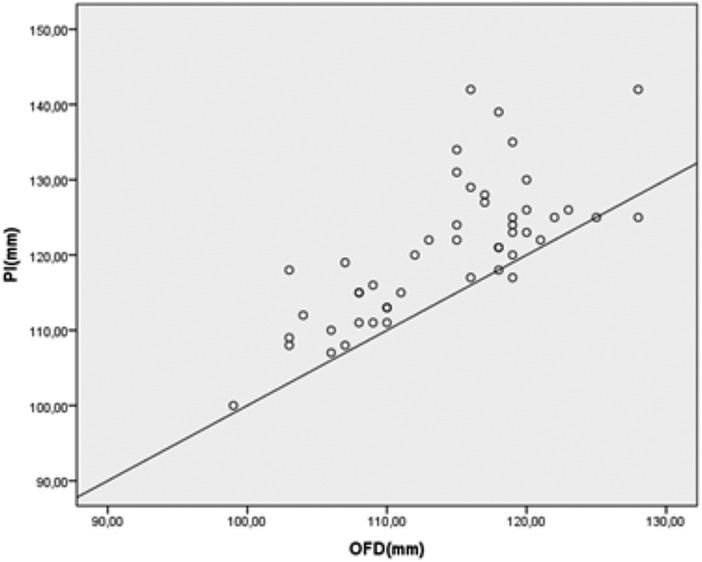
Figure 3. Pfannensitel incision and OFD values of the study population shown in a Scatter Plot Graphic. PI, pfannenstiel incision; OFD, occipitofrontal diameter.
In the study, any correlation was not found between the Pfannenstiel incision length and features, including maternal age, body mass index (BMI), fetal weight, and fetal ultrasonographic measurements (Table 4).
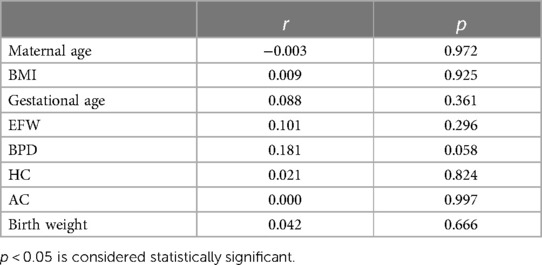
Table 4. The correlation analysis of Pfannenstiel incision–OFD difference according to the demographic, clinic, and ultrasound parameters.
There was no statistical difference in terms of fetal ultrasonographic measurements, including OFD, BPD, HC, as well as fetal weight, neonatal outcomes, and also maternal features between the ≤1 cm group (n = 90) and >1 cm group (n = 19) (Table 5).
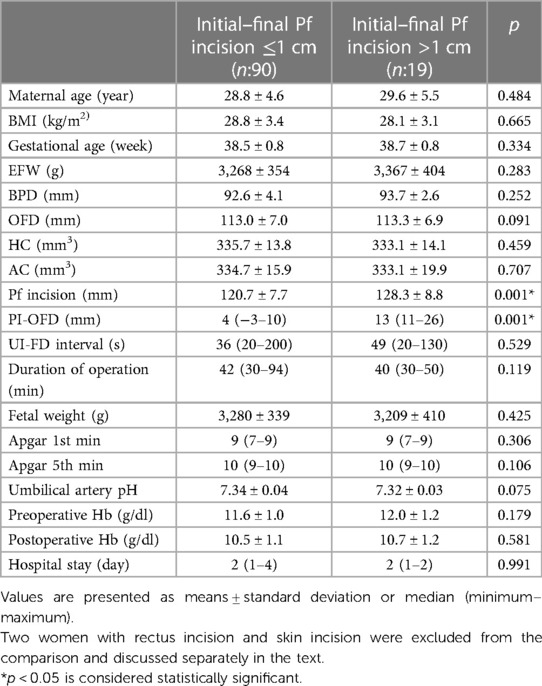
Table 5. Comparison of maternal, fetal, and perioperative features of groups between the initial and final Pf incision ≤1 and >1 cm.
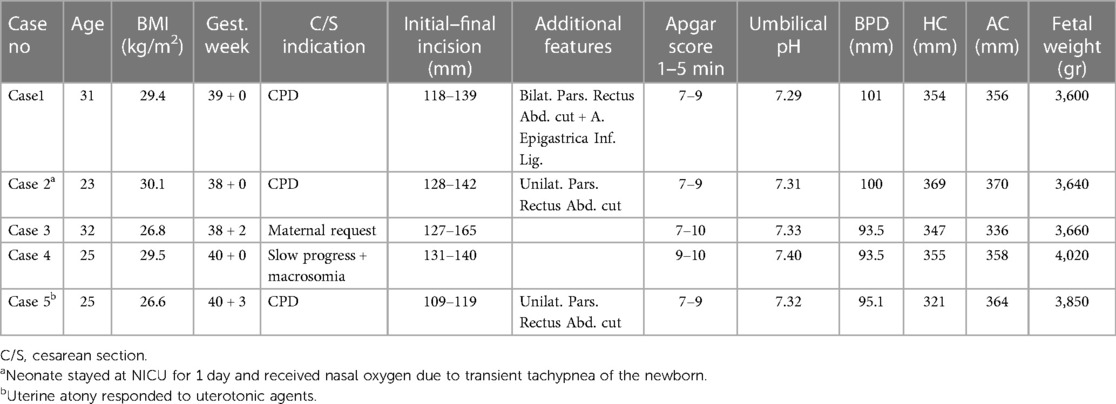
In five cases (4.4%), the Pfannenstiel incision arranged according to the fetal OFD had to be extended with scissors between 10 and 38 mm and accepted as a technique failure. In three of these five women, the rectus abdominis muscle was partially cut to deliver the fetal head before Pfannenstiel skin incision extension. In two women, only skin incisions were extended to deliver the baby.
In the failed cases (n = 5), the mean fetal measurements, including fetal weight, were higher than the mean measurements of successful cases (n = 109) [BPD (96.7 ± 3.7 vs. 92.8 ± 3.9; p = 0.030), OFD (115.8 ± 7.1 vs. 122.85 ± 8.9; p = 0.042), HC (335 ± 13 vs. 349 ± 17; p = 0.032), abdominal circumflex (AC) (334 ± 16 vs. 357 ± 12; p = 0.003), fetal weight 3,265 (2,400–4,065) vs. 3,660 (3,600–4,200); p = 0.003] (Table 6).
In seven women, the rectus abdominis muscle was partially cut (unilaterally or bilaterally) without the need for an extension of the Pfannenstiel skin incision. There was no epigastric inferior artery ligation performed. When we look at the rectus-cut and without-cut women, maternal and fetal features, including fetal head diameters and fetal weight, were similar in both groups. Due to difficulty during cesarean delivery of the fetus in this seven women, uterine incision to fetal delivery time was longer [36 s (20–130) vs. 128 s (28–195); p = 0,001]. Despite 5-min Apgar scores and umbilical pH levels of the newborns being statistically significantly lower than the women without rectus-cut cases [5-min Apgar scores 10 (8–10) vs. 9 (9–10), p = 0.013; umbilical pH: 7.34 ± 0.03 vs. 7.28 ± 0.07; p = 0.001], neither fetal hypoxia nor fetal acidosis was encountered in the cases.
Three postpartum hemorrhages due to uterine atony were encountered among the study population. One was excluded from the study because of the skin incision extension during the Bakri balloon implementation due to uterine atony. In the other one, the B-Lynch compression suture was performed without needing to extend the skin incision and therefore was included in the study. The last one responded to uterotonic treatment. Blood and blood products were transfused in both. Neither endometritis nor wound infection was encountered in this study.
No neonatal asphyxia was encountered among the newborns. Five babies were followed up at the neonatal intensive care unit (NICU). One was diagnosed with Hirschsprung disease and kept in NICU for 20 days. One neonate was admitted to the NICU due to hypoglycemia and stayed for 3 days. Three newborns were admitted to the NICU and received treatment with nasal oxygen ± continuous positive airway pressure (nCPAP) due to transient tachypnea of the newborn (TTN), with a stay duration ranging from 1 to 6 days. No endotracheal intubation was needed for any newborn.
Discussion
In this study, in 109 out of 114 women, cesarean delivery was successfully (95.6%) performed with minimal margins of error via the obtained Pfannenstiel skin incision length according to the ultrasonographic measurement of the OFD of the fetal head. In 90 out of 109 women (82.5%), the difference between the skin incision performed according to the OFD and the final Pfannenstiel incision was maintained within 1 cm.
Our study results showed that if the Pfannenstiel incision is adjusted according to the fetal OFD, the incision length will be approximately 12 cm. Cahana et al. (12) classified the Pfannenstiel incision lengths of the women with repeated CD as short <14 cm, medium = 14–17 cm, and long >17 cm. In their study, among 545 women, approximately two-thirds of Pfannenstiel incisions were between 14 and 17 cm (12). Recently, a multicenter study from the USA among 1,916 women reported the mean Pfannenstiel incision length as 15.3 ± 2.3 cm. The incision length was less than 14.5 cm in one-third of the women, while in one-quarter of the women, the incision length was measured at more than 16.5 cm (13). Unlike the above studies from the USA, Giacalone et al. (9) measured the Pfannenstiel incision as 11.7 ± 1.4 cm among 54 women in France, which also proves that surgeons from different regions of the world have a distinct tendency for the cesarean incision lengths.
The question is whether a universal incision length in clinical practice can be applied to all women worldwide. Studies showed that European newborns’ fetal heads had larger head circumferences than South Asian and Middle East/North African ethnicities (20). In contrast, Asian newborns were smaller and had lower birthweight than ethnic Europeans (21). Moreover, one's anthropometric features and socioeconomic factors can differ from another even in the same ethnicity, affecting fetal biometric measurements and fetal growth (22–25). It has been shown that fetal head size was influenced by features such as maternal age, height, weight, parity, and fetal gender; however, AC and femur length (FL) were both correlated with maternal weight (25). Therefore, a 15 cm Pfannenstiel incision length, as suggested previously (7, 8), might be too wide for Asian women (or women with similar body types) or any women carrying a baby with average dimensions.
The significant advantage of the current technique is: it can be applied to women of all kinds of body types and ethnicities.
Extending the skin incision during fetal head delivery was an accepted failure of the technique in this study. In five (4.4%) out of 114 cases, the surgeons needed to extend the skin incisions, where rectus abdominis muscle was cut partially in three cases. Reasons for the difficulty of delivering the fetal head can be an unengaged or floating head as well as tight or contracted rectus abdominis (probably regional anesthesia effect), maternal features, or the fetal head size and fetal weight.
The number of failed cases is relatively few in the study; however, we may speculate that in women with high BPD, HC, and AC measurements (97th percentile), OFD cannot accurately estimate the Pfannenstiel skin incision.
Another reason for unsuccessful attempts may be some aggressive efforts during cesarean delivery or any degree of fetal head extension due to maneuvers that can cause difficult delivery and failure of the current technique.
In seven out of 114 women (6.1%), delivery of the fetuses was difficult during the operation; therefore, the rectus abdominis muscle was partially cut (unilateral, n = 3; bilateral, n = 4) without extension of the skin incision. Tight or too contracted rectus abdominis (especially with regional anesthesia) can cause difficult delivery of the fetus during cesarean delivery. They may require excessive maternal fundal pressure applied by the assistance or, in some cases, the rectus abdominis muscle can be cut to deliver the baby. Nevertheless, in wider Pfannenstiel incisions, despite the rectus abdominis muscle being tight or contracted, the opening of the incision may allow the muscle sheets to be retracted by the fingers of the assistants or instruments. However, in the current technique, since the Pfannenstiel incision was relatively shorter, the rectus abdominis muscle must be partially cut (unilateral or bilateral) to deliver the baby's head. There are no complications due to a partial rectus muscle cut; clinical and isokinetic testing for abdominal wall strength showed that the rectus abdominis muscle cut has no harm to the mother compared with the Pfannenstiel incision alone (9). In our study, the time interval between the uterine incision and delivery of the fetus was prolonged, and 5-min Apgar scores and umbilical pH levels were lower in the rectus-cut cases; however, neither fetal hypoxia nor fetal acidosis was encountered.
Apart from the time-honored Pfannenstiel incision for CD, some modifications were made in terms of the higher level of skin incision (Joel–Cohen incision) with being more straight and its modification with fewer usage of sharp instruments, called Misgav–Ladach method (26). These techniques provided shorter operation time and faster recovery with fewer wound infections (27). Nevertheless, in these techniques, the skin incision was several centimeters higher (above the underwear or bikini level) than the original Pfannenstiel incision; moreover, it needs at least 15–17 cm in length (27), which means that these techniques’ abdominal incision looks wider than ours and much higher in level than the original Pfannenstiel incision. Joel–Cohen and Misgav–Ladach techniques did not meet the esthetic expectations of many women (28); however, Belci et al. showed better long-term postoperative results (5 years after CS) in terms of the neuropathic and chronic pain and the cosmetic appearance of the scar in a comparative study (29).
A modified version of the Misgav–Ladach method, which uses the same principles as the original technique but makes the abdominal incision at the same level as the Pfannenstiel incision, gained popularity among obstetricians (28, 30). However, contrary to our modification of the Pfannenstiel incision, all these above techniques focused on the incision level or the surgical techniques rather than the incision length.
Strength and limitations
The current study is the first to investigate the Pfannenstiel incision length estimation according to the ultrasonographic measurement of the OFD of the fetal head and define a novel technique. The number of cases and design are the main limitations of the study. Only three surgeons used this novel technique. The length of the incision was the primary outcome; therefore, esthetic evaluation was not performed among the women. Also, long-term maternal outcomes of the current technique were not evaluated in this study.
Conclusion
According to our study findings, the Pfannenstiel incision can be adjusted according to the OFD with minimal margins of error. This modification allows the Pfannenstiel incision length to be kept as fetal head OFD length and may avoid unnecessarily wide incisions providing better cosmetic results without newborn issues or problems in selected patients. Further studies are needed to understand this technique better.
Data availability statement
The raw data supporting the conclusions of this article are available upon request to the corresponding author.
Ethics statement
This interventional pilot study was approved by the Yakın Dogu University Ethics Committee (30.09.2021, Number: YDU 2021/95-1398). This study was carried out according to the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The patents/participants provided their written informed consent to participate in this study.
Author contributions
BK invented the surgical technique, designed and carried out the study, performed the surgical procedures, followed up with the patients, interpreted the data, wrote the first draft of the manuscript, and finalized the paper. OO and AO carried out the study, performed the surgical procedures, followed up with the patients, and contributed to the first draft of the paper. AT performed the statistical analyses, revised the manuscript critically for important intellectual content, and finalized the paper. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1227026/full#supplementary-material
Supplementary Videos S1, S2
Demonstration of the surgical technique: Pfannenstiel skin incision according to the fetal occipitofrontal diameter during cesarean delivery (Pfannenstiel skin incision with Kaya modification).
Abbreviations
OFD, occipitofrontal diameter; BPD: biparietal diameter; HC, head circumflex; EFW: estimated fetal weight; FL, femur length; CD, cesarean delivery.
References
1. Kehrer FA. Ueber ein modificirtes verfahren beim kaiserschnitt. Arch Gynaek. (1882) 19:177–209. doi: 10.1007/BF01886653
3. Kerr JMM. The technic of caesarean section with special reference to the lower uterine segment incision. Am J Obstet Gynaecol. (1926) 12:726.
4. Pfannenstiel HJ. Uber die vortheile des suprasymphysaren fascien-querschnitts fur die gynakolodischen koliotomien zugleich ein beitag zu der iindikationsstellung der operationswege. Samml Klin Votr Lepzig. (1900) 268:1735–56.
5. Kisielinski K, Conze J, Murken AH, Lenzen NN, Klinge U, Schumpelick V. The pfannenstiel or so-called “bikini cut": still effective more than 100 years after first description. Hernia. (2004) 8(3):177–81. doi: 10.1007/s10029-004-0210-0
6. Cundiff GW, Gomel V. Incisions and closures. In: Yeomans ER, Hoffman BL, Gilstrap III LC, Gary Cunningham F, editors. Cunningham and Gilstrap's operative obstetrics. 3rd edn. New York: McGraw-Hill Education (2017). p. 49–55.
7. Ayers JW, Morley GW. Surgical incision for cesarean section. Obstet Gynecol. (1987) 70(5):706–8.2958727
8. Finan MA, Mastrogiannis DS, Spellacy WN. The “Allis” test for easy cesarean delivery. Am J Obstet Gynecol. (1991) 164(3):772–5. doi: 10.1016/0002-9378(91)90512-p
9. Giacalone PL, Daures JP, Vignal J, Herisson C, Hedon B, Laffargue F. Pfannenstiel versus Maylard incision for cesarean delivery: a randomized controlled trial. Obstet Gynecol. (2002) 99(5 Pt 1):745–50. doi: 10.1016/s0029-7844(02)01957-9
10. De Vivo A, Mancuso A, Giacobbe A, Priolo AM, De Dominici R, Maggio Savasta L. Wound length and corticosteroid administration as risk factors for surgical-site complications following cesarean section. Acta Obstet Gynecol Scand. (2010) 89(3):355–9. doi: 10.3109/00016340903568175
11. Nagaria T, Kujur A, Thakur N. Incision length: an emerging risk factors for surgical-site infection following cesarean section. Int J Reprod Contracept Obstet Gynecol. (2017) 6(5):1829–33. doi: 10.18203/2320-1770.ijrcog20171566
12. Cahana RL, Carvalho B, Siaulys MM, Corradini BR, Granot M. Influence of surgical incision length on chronic post-cesarean pain. [Conference presentation abstract] in the anesthesiology annual meeting of American society of anesthesiologists. Boston, USA. (2017). p. 43029.552083–43029.635417. 21–25 October.
13. Subramaniam A, Jauk V, Saade G, Boggess K, Longo S, Clark EAS, et al. The association of cesarean skin incision length and postoperative wound complications. Am J Perinatol. (2020) 39(5):539–45. doi: 10.1055/s-0040-1716889
14. Nicholls-Dempsey L, Abenhaim H. Cesarean section incision length and post-operative pain [34R]. Obstet Gynecol. (2019) 133:200S. doi: 10.1097/01.AOG.0000559159.37364.63
15. Luijendijk RW, Jeekel J, Storm RK, Schutte PJ, Hop WC, Drogendijk AC, et al. The low transverse Pfannenstiel incision and the prevalence of incisional hernia and nerve entrapment. Ann Surg. (1997) 225(4):365–9. doi: 10.1097/00000658-199704000-00004
16. Loos MJ, Scheltinga MR, Mulders LG, Roumen RM. The ‘Pfannenstiel’ approach as a source of chronic pain. Obstet Gynecol. (2008) 111:839–46. doi: 10.1097/AOG.0b013e31816a4efa
17. Loos MJ, Scheltinga MR, Roumen RM. Surgical management of inguinal neuralgia after a low transverse pfannenstiel incision. Ann Surg. (2008) 248(5):880–5. doi: 10.1097/SLA.0b013e318185da2e
18. Ishibashi S, Takeuchi H, Fujii K, Shiraishi N, Adachi Y, Kitano S. Length of laparotomy incision and surgical stress assessed by serum IL-6 level. Injury. (2006) 37(3):247–51. doi: 10.1016/j.injury.2005.08.008
19. Kaya B, Guralp O, Daglar K, Tuten A, Demirol A, Yayci E, et al. Extra-abdominal removal of placenta during cesarean section: a prospective randomized controlled trial of a novel technique. J Perinat Med. (2016) 44(5):557–65. doi: 10.1515/jpm-2015-0330
20. Sletner L, Kiserud T, Vangen S, Nakstad B, Jenum AK. Effects of applying universal fetal growth standards in a Scandinavian multi-ethnic population. Acta Obstet Gynecol Scand. (2018) 97(2):168–79. doi: 10.1111/aogs.13269
21. Cheng Y, Leung TY, Lao T, Chan YM, Sahota DS. Impact of replacing Chinese ethnicity-specific fetal biometry charts with the INTERGROWTH-21(st) standard. BJOG. (2016) 123(Suppl 3):48–55. doi: 10.1111/1471-0528.14008
22. Makgoba M, Savvidou MD, Steer PJ. The effect of maternal characteristics and gestational diabetes on birthweight. BJOG. (2012) 119(9):1091–7. doi: 10.1111/j.1471-0528.2012.03388.x
23. Leary S, Fall C, Osmond C, Lovel H, Campbell D, Eriksson J, et al. Geographical variation in relationships between parental body size and offspring phenotype at birth. Acta Obstet Gynecol Scand. (2006) 85(9):1066–79. doi: 10.1080/00016340600697306
24. Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. (2010) 39(3):263–72. doi: 10.1016/j.amepre.2010.05.012
25. Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. (2009). doi: 10.1056/NEJMoa0803267
26. Holmgren G, Sjöholm L, Stark M. The Misgav Ladach method for cesarean section: method description. Acta Obstet Gynecol Scand. (1999) 78:615–21.10422908
27. Vitale SG, Marilli I, Cignini P, Padula F, D'Emidio L, Mangiafico L, et al. Comparison between modified Misgav-Ladach and Pfannenstiel-Kerr techniques for cesarean section: review of literature. J Prenat Med. (2014) 8(3–4):36–41.26265999
28. Xavier P, Ayres-De-Campos D, Reynolds A, Guimarães M, Costa-Santos C, Patrício B. The modified Misgav-Ladach versus the Pfannenstiel-Kerr technique for cesarean section: a randomized trial. Acta Obstet Gynecol Scand. (2005) 84(9):878–82. doi: 10.1111/j.0001-6349.2005.00631.x
29. Belci D, Di Renzo GC, Stark M, et al. Morbidity and chronic pain following different techniques of caesarean section: a comparative study. J Obstet Gynaecol. (2015) 35(5):442–6. doi: 10.3109/01443615.2014.968114
Keywords: cesarean delivery, Pfannenstiel incision, incision length, occipitofrontal diameter, Aesthetic cesarean incision
Citation: Kaya B, Ozay OE, Ozay AC and Tüten A (2023) Can the Pfannenstiel skin incision length be adjusted according to the fetal head during elective cesarean delivery?. Front. Surg. 10:1227338. doi: 10.3389/fsurg.2023.1227338
Received: 23 May 2023; Accepted: 6 September 2023;
Published: 26 September 2023.
Edited by:
Andrea Tinelli, Xi'an Jiaotong University, ChinaReviewed by:
Michael Stark, New European Surgical Academy (NESA), GermanyDragan Belci, General Hospital Pula, Croatia
© 2023 Kaya, Ozay, Ozay and Tüten. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baris Kaya mdbariskaya@gmail.com
†ORCID Baris Kaya orcid.org/0000-0002-2773-1132
 Baris Kaya
Baris Kaya Ozlen Emekci Ozay2
Ozlen Emekci Ozay2  Ali Cenk Ozay
Ali Cenk Ozay