Effects of duration of long-acting GnRH agonist downregulation on assisted reproductive technology outcomes in patients with adenomyosis: a retrospective cohort study
- 1Center for Reproductive Medicine, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
- 2Research Unit of Gametogenesis and Health of ART-Offspring, Chinese Academy of Medical Sciences (No. 2021RU001), Jinan, Shandong, China
- 3Key Laboratory of Reproductive Endocrinology of Ministry of Education, Shandong University, Jinan, Shandong, China
- 4Shandong Key Laboratory of Reproductive Medicine, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 5Shandong Provincial Clinical Research Center for Reproductive Health, Jinan, Shandong, China
- 6Shandong Technology Innovation Center for Reproductive Health, Jinan, Shandong, China
- 7National Research Center for Assisted Reproductive Technology and Reproductive Genetics, Shandong University, Jinan, Shandong, China
- 8Center for Reproductive Medicine, The Second Hospital of Shandong University, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
- 9Shanghai Key Laboratory for Assisted Reproduction and Reproductive Genetics, Shanghai, China
- 10Center for Reproductive Medicine, Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
Objectives: To elucidate the relationship between long-acting GnRH agonist (GnRHa) downregulation and assisted reproductive technology (ART) outcomes and identify the optimal duration of downregulation in patients with adenomyosis.
Design: Retrospective cohort study.
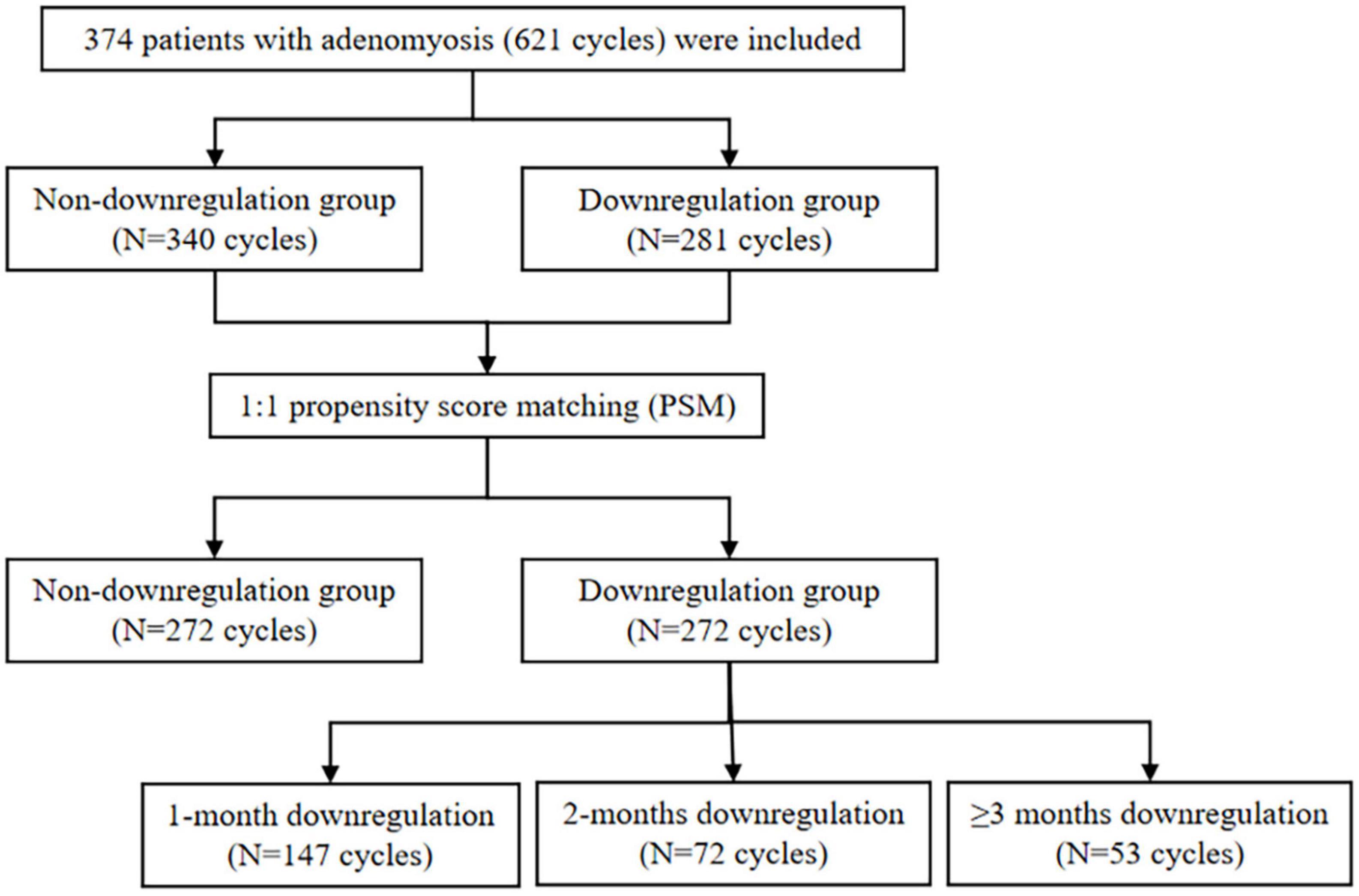
Participants: The study was designed to evaluate ART outcomes in adenomyosis patients with and without GnRHa downregulation between January 2016 and December 2020. A total of 374 patients with adenomyosis (621 cycles) were included with 281 cycles in downregulation group versus 340 cycles in non-downregulation group. After 1:1 propensity score matching (PSM), a sample size of 272 cycles in each group was matched. The matched downregulation group was further divided into 1-month (147 cycles), 2-months (72 cycles), and ≥3 months downregulation (53 cycles) subgroups. Stratification analysis was conducted on pregnancy outcomes in 239 fresh embryo transfer (ET) cycles and 305 frozen embryo transfer (FET) cycles.
Results: The downregulation group had larger mean diameter of initial uterus and higher proportion of severer dysmenorrhea compared to non-downregulation group. The pregnancy-related parameters in GnRHa downregulation group were similar to those in non-downregulation group, except for higher late miscarriage rate (MR) (13.4% vs. 3.1%, P = 0.003). The subgroup comparisons in fresh ET cycles indicated that implantation rate (75.0% vs. 39.2%, P = 0.002), biochemical pregnancy rate (91.7% vs. 56.0%, P = 0.036) and clinical pregnancy rate (83.3% vs. 47.0%, P = 0.016) could be improved by prolonged GnRHa downregulation (≥3 months), whereas late MR was difficult to be reversed (30.0% vs. 3.2%, P = 0.017). In FET cycles, higher MR (53.6% vs. 29.9%, P = 0.029; 58.8% vs. 29.9%, P = 0.026) and lower live birth rate (18.8% vs. 34.1%, P = 0.023; 17.1% vs. 34.1%, P = 0.037) were observed in the 1-month and ≥3 months downregulation group, while no differences were found in the 2-months downregulation group compared to the non-downregulation group.
Conclusion: In patients with severer adenomyosis, long-acting GnRHa downregulation might be correlated with improved ART outcomes. In fresh ET cycles, prolonged downregulation (≥3 months) might be beneficial to improve live birth rate, which needed to be verified by further study with larger sample. In FET cycles, the optimal duration of downregulation was not certain and still needed further exploration.
Key points
1. Firstly, we adopted PSM approach to eliminate the influence of confounding factors and enhance the comparability between the downregulation group and non-downregulation group.
2. Secondly, subgroup analysis was performed to evaluate the dose-response relationship between the duration of long-acting GnRHa downregulation and pregnancy outcomes.
3. Thirdly, stratification analysis was used to evaluate the different downregulation strategies in fresh ET and FET cycles.
4. The study was single-center, retrospective, and the sample size was limited.
Introduction
Adenomyosis, an estrogen-dependent disease, is characterized by the invasion of endometrial gland and stroma into the myometrium, which contributes to uterine enlargement, abnormal uterine bleeding, chronic pelvic pain and infertility (1–3). The performances of adenomyosis by ultrasound and magnetic resonance imaging (MRI) are manifold and elusive (4). In the field of assisted reproductive technology (ART), adenomyosis was a non-negligible factor for patients with infertility, and its prevalence in women ≥ and <40 years old were respectively 29.7% and 22.0% (5). One previous meta-analysis indicated that implantation rate (IR), clinical pregnancy rate (CPR) and live birth rate (LBR) significantly decreased in patients with adenomyosis compared to non-adenomyosis patients receiving in vitro fertilization (IVF) treatment (6). Additionally, adenomyosis might increase the occurrence of maternal and neonatal complications, such as preterm birth, preeclampsia, small for gestational age, preterm premature rupture of membranes, postpartum hemorrhage and neonatal intensive care unit admission rate (7–9). The adverse effects of adenomyosis on clinical outcomes might be associated with disruptive endometrial receptivity, aberrant tubal transport, distorted uterine cavity and irregular uterine contractility (10–12).
Long-acting GnRH agonist (GnRHa) is usually used in patients with adenomyosis receiving ART treatment, because it can induce and maintain a hypoestrogenic state by suppressing gonadotropin secretion (13). Moreover, it can induce apoptosis of ectopic endometrium, relieve inflammation reaction and reduce aberrant angiogenesis in adenomyotic lesions, which are beneficial to reduce the uterine size and relieve clinical symptoms (14, 15). Therefore, long-acting GnRHa downregulation was utilized not only before controlled ovarian stimulation (COS) in fresh embryo transfer (ET) cycles but also before endometrial preparation in frozen embryo transfer (FET) cycles. However, there was continuing debating on the effect of long-acting GnRHa downregulation on ART outcomes in patients with adenomyosis. Two retrospective studies elucidated that ultralong GnRHa downregulation protocol improved CPR compared to long and short GnRHa protocols in patients with adenomyosis (16, 17), however, Lan et al.’ (18) study did not support the improvement of CPR. Similarly, in the FET cycles, Niu et al.’ (19) study demonstrated that long-acting GnRHa downregulation followed by hormone replacement therapy (HRT) protocol significantly improved CPR in adenomyosis patients compared with the sole HRT protocol, but no consistent conclusion was supported by another two studies (20, 21). Besides the divergence of the role of long-acting GnRHa downregulation, the duration of downregulation in patients with adenomyosis undergoing ART was also disputable. Previous studies verified that prolonged GnRHa treatment reduced uterine volume and increased uterine elasticity in patients with adenomyosis, which might improve pregnancy outcomes (22–24), whereas the optimum duration of downregulation still needed further exploration.
Consequently, we designed this retrospective study to elucidate the relationship between long-acting GnRHa downregulation and pregnancy outcomes and try to identify the optimal duration of downregulation in patients with adenomyosis undergoing ART treatment.
Materials and methods
Study design and population
This retrospective cohort study included patients with adenomyosis who underwent ART at the Center for Reproductive Medicine, Shandong University from January 2016 to December 2020 with the follow-up time of FET up to June 2022. The adenomyosis was diagnosed by transvaginal ultrasound (TVS), which was reviewed independently by two sonographers experienced in gynecologic imaging. The diagnostic standard coincided with the Morphological Uterus Sonographic Assessment (MUSA) statement (25). The typical sonographic features were enlarged uterus with spherical appearance or asymmetrical thickening of myometrium, accompanying with or without echogenic lines and buds under the endometrium, hyperechoic islands, translesional vascularity, fan-shaped shadowing, cystic echogenicity, irregular or interrupted junctional zone (26). Patients with uterine malformation, chromosomal abnormality or preimplantation genetic testing were excluded from the study. The downregulation was defined as the usage of long-acting GnRHa before ET, which might range from 1 to 6 months. Conversely, the absence of long-acting GnRHa was defined as non-downregulation. According to the GnRHa duration, the downregulation group was further divided into 1-month downregulation, 2-months downregulation, and ≥3 months downregulation subgroups.
Controlled ovarian stimulation
The long-acting GnRHa downregulation was usually used in patients with severer adenomyosis with normal ovarian reserve. The usage of other protocols were decided according to patient’s comprehensive situations. In the ultra-long protocol, patients received the first injection of long-acting GnRHa (Triptorelin Acetate for Injection, 3.75 mg, Ipsen Pharma Biotech, France; Leuprorelin Acetate Microspheres for Injection, 3.75 mg, Lizhu, China; Goserelin Acetate Sustained-Release Depot, 3.6 mg, AstraZeneca, UK) on day 2 or 3 of the menstrual cycle, and the comprehensive evaluation of serum hormone levels, the diameter of follicles and uterine size 28 days later was carried out to determine whether long-acting GnRHa downregulation continued. The standard of pituitary downregulation was defined as low levels of serum luteinizing hormone (LH, < 5 IU/L) and estradiol (E2, < 50 pg/ml), thin endometrial thickness (<5 mm), the diameters of follicles <8 mm in bilateral ovary and no existing of functional cysts. After 28 days of the last long-acting GnRHa injection, gonadotropin (Gonal F, Merck Serono, Switzerland; Puregon, MRK, China; Lishenbao, Lizhu, China) 150–300 IU daily was administered for subsequent COS.
The starting doses of gonadotropin were determined by comprehensive consideration of age, body mass index (BMI), ovarian reserve function including parameters of AFC, anti-mullerian hormone (AMH), and serum follicle stimulating hormone (FSH) level. Adjuvant drugs, such as recombinant human lutropin α, metformin and growth hormone, were added according to the principle of individualized treatment. When at least two leading follicles reached 18 mm or greater, 8,000–10,000 IU of urinary human chorionic gonadotropin (hCG, Livzon Pharmaceutical Group. Inc., Zhuhai, China) was administered intramuscularly to trigger oocyte maturation. The dosage and timing of hCG were confirmed basing on the number of dominant follicles, serum E2 levels, BMI and ovarian reserve function. Oocyte retrieval guided by TVS was carried out 36–38 h later. Oral dydrogesterone tablet (Duphaston, Abbott Biologicals B.V., Netherlands) 10 mg twice daily and vaginal progesterone gel (Crinone gel, Merck Serono, Switzerland) 90 mg once daily were administered as luteal phase support. IVF or intracytoplasmic sperm injection (ICSI) was selected in the procedure of fertilization depending on sperm quality. Two high-quality cleavage-stage embryos on day 3 or one blastocyst on day 5 after oocyte retrieval were transferred into the uterus under the guidance of abdominal ultrasound. The high-quality embryos were defined as 2PN (pronuclear)-derived embryos with 7–10 cells and scores ≥ 3 on day 3 and ≥ 4BC on day 5 (27). If fresh ET was canceled or the remaining embryos were present, the eligible embryo would be frozen. The whole embryo freezing was recommended, such as varian hyperstimulation syndrome, elevated serum progesterone on hCG trigger day or hydrosalpinx. Other protocols of COS without long-acting GnRHa had been described in previous studies published by our center (28, 29).
Endometrial preparation in FET cycles
Patients undergoing GnRHa downregulation combined with HRT received the first injection of 3.75 mg long-acting GnRHa on day 2 or 3 of the menstrual cycle. The results of serum hormone levels and sonographic evaluation 28 days later determined the continuation of long-acting GnRHa. About 28 days after last injection of long-acting GnRHa, HRT was performed for endometrial preparation. Oral estradiol valerate (Progynova; Bayer AG, Germany) was administrated in a dose-escalating method, 6 mg/day for the first 5 days and subsequently 8 mg/day for the next 5 days. After 10 days, 8 mg/day might be continued for 3–4 days according to the comprehensive assessment of the endometrial thickness, and serum hormone levels. When endometrial thickness reached at least 7 mm, oral dydrogesterone tablet 20 mg twice daily and vaginal progesterone soft capsules (Utrogestan, Besins, Belgium) 200 mg once daily were used to transform endometrium. One frozen-thawed blastocyst was transferred into the uterus under the guidance of abdominal ultrasound 5–6 days after the addition of progesterone. After ET, progesterone was continued for luteal phase support. Other protocols for endometrial preparation in FET cycles have been described in the previous study (30).
Observational parameters and outcome variables
Observational parameters included basic characteristics of patients, the mean diameter of initial uterus, the history of dysmenorrhea and IVF-related parameters. The mean diameter of initial uterus was calculated as the average of long and wide diameters in longitudinal section by TVS between day 2 and day 5 of the menstrual cycle. The dysmenorrhea was classified into none, mild, moderate and severe degrees according to the verbal multidimensional scoring system, which mainly depended on subjective feelings of patients (31). The primary pregnancy outcome was LBR, and the secondary pregnancy outcomes included CPR, IR, biochemical pregnancy rate (BPR), miscarriage rate (MR), early MR and late MR. The definitions of these outcomes based on the International Glossary on Infertility and Fertility Care (32). The serum β-hCG level was examined 14 days after ET. Biochemical pregnancy was defined as a serum β-hCG level ≥ 10 IU/L. Clinical pregnancy was defined as the presence of one or more gestational sacs confirmed by TVS including ectopic pregnancy. Miscarriage was defined as pregnancy loss <28 gestational weeks. Early miscarriage occurred <12 gestational weeks, and late miscarriage occurred ≥12 gestational weeks. Live birth was defined as delivery of at least one viable infant ≥28 gestational weeks. IR was defined as the ratio of total numbers of gestational sac confirmed by TVS to total numbers of transferred embryos.
Statistical analysis
A 1:1 propensity score matching (PSM) approach using nearest neighbor matching (caliper value = 0.03) was applied to deal with the confounding factors and enhance comparability between groups on R software using “MatchIt” package. Matching variables included age, BMI, duration of infertility, basal FSH, AFC, AMH, the proportion of primary infertility, endometriosis and previous gynecological surgery. Further subgroup analysis was performed using the PSM dataset, which compared pregnancy outcomes of 1-month, 2-months, and ≥3 months downregulation subgroups in the non-downregulation group. Stratification analysis was conducted on pregnancy outcomes in fresh ET and FET cycles. Shapiro–Wilk test was utilized to test the normality of continuous variables. Median (25th–75th percentile) was utilized to describe non-normality distribution variables. Frequencies (percentages) were utilized to describe categorical variables. Continuous variables with non-normality distribution were compared between groups by the Mann–Whitney U test. Categorical variables were compared between groups by χ2 test or Fisher’s exact test. Bonferroni method was used to carry out subgroups comparisons. P < 0.05 was considered as statistically significant. All statistical analysis were conducted by SPSS 25.0 (SPSS, Inc., Chicago, IL, USA) and R software 4.2.0.
Results
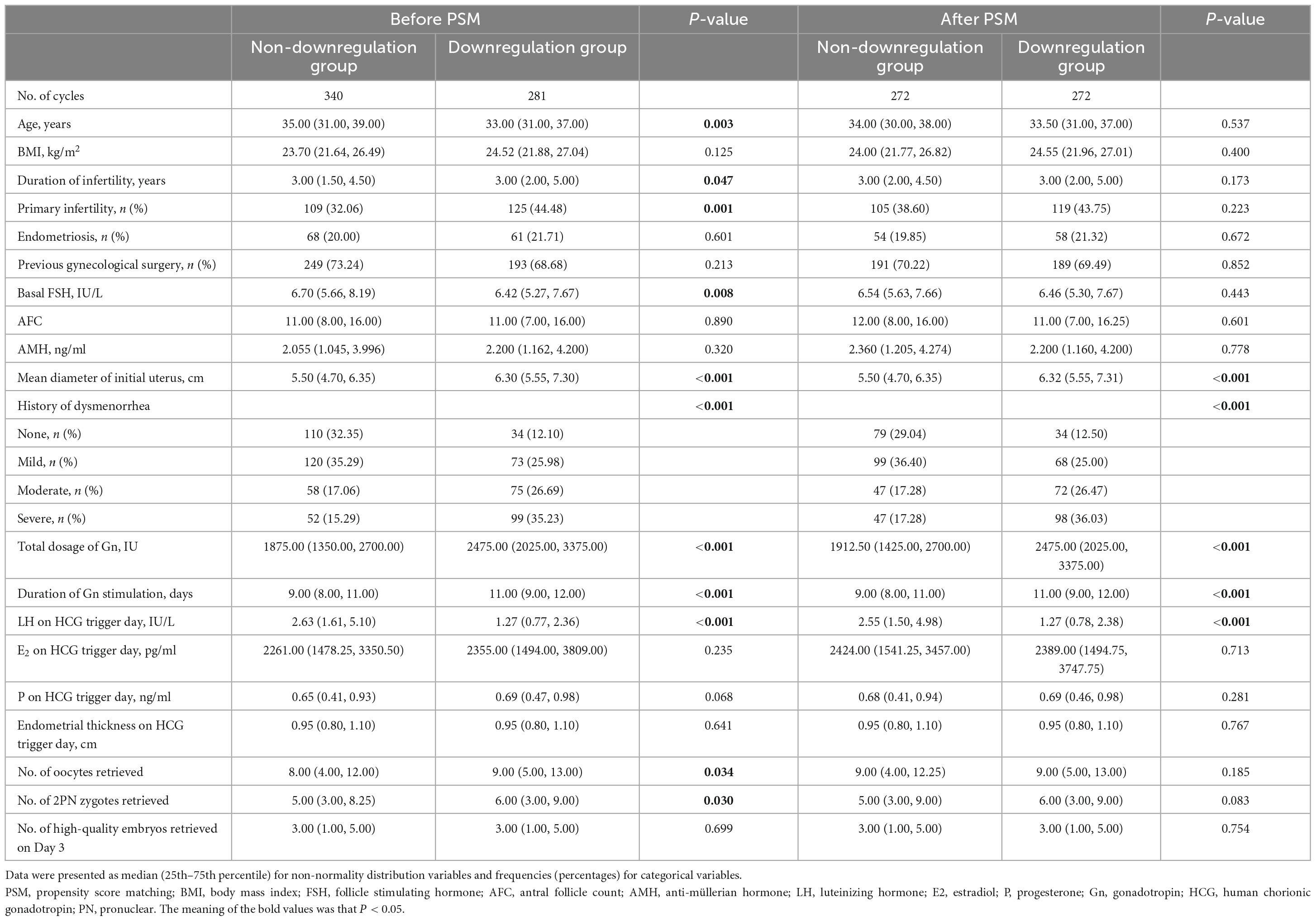
A total of 374 patients with adenomyosis (621 cycles) were included with 281 cycles in downregulation group versus 340 cycles in non-downregulation group. PSM was used to balance the demographical bias between two groups. The flowchart of the study was shown in Figure 1. The characteristics of the study population before and after PSM were shown in Table 1. Before PSM, the downregulation group had younger age, longer duration of infertility, higher proportion of primary infertility and lower basal FSH compared to the non-downregulation group. After PSM, these factors were well balanced. Ultimately it involved a matched sample size with 272 cycles in each group. Except for these matching factors, the downregulation group had larger mean diameter of initial uterus (6.32 vs. 5.50 cm, P < 0.001) and higher proportion of severe dysmenorrhea (36.03% vs. 17.28%, P < 0.001) compared to the non-downregulation group. The pregnancy outcomes of two groups after PSM were shown in Table 2. No differences were found in the IR, BPR, CPR, MR, early MR, and LBR, while late MR in the downregulation group was significantly higher than the non-downregulation group (13.4% vs. 3.1%, P = 0.003).
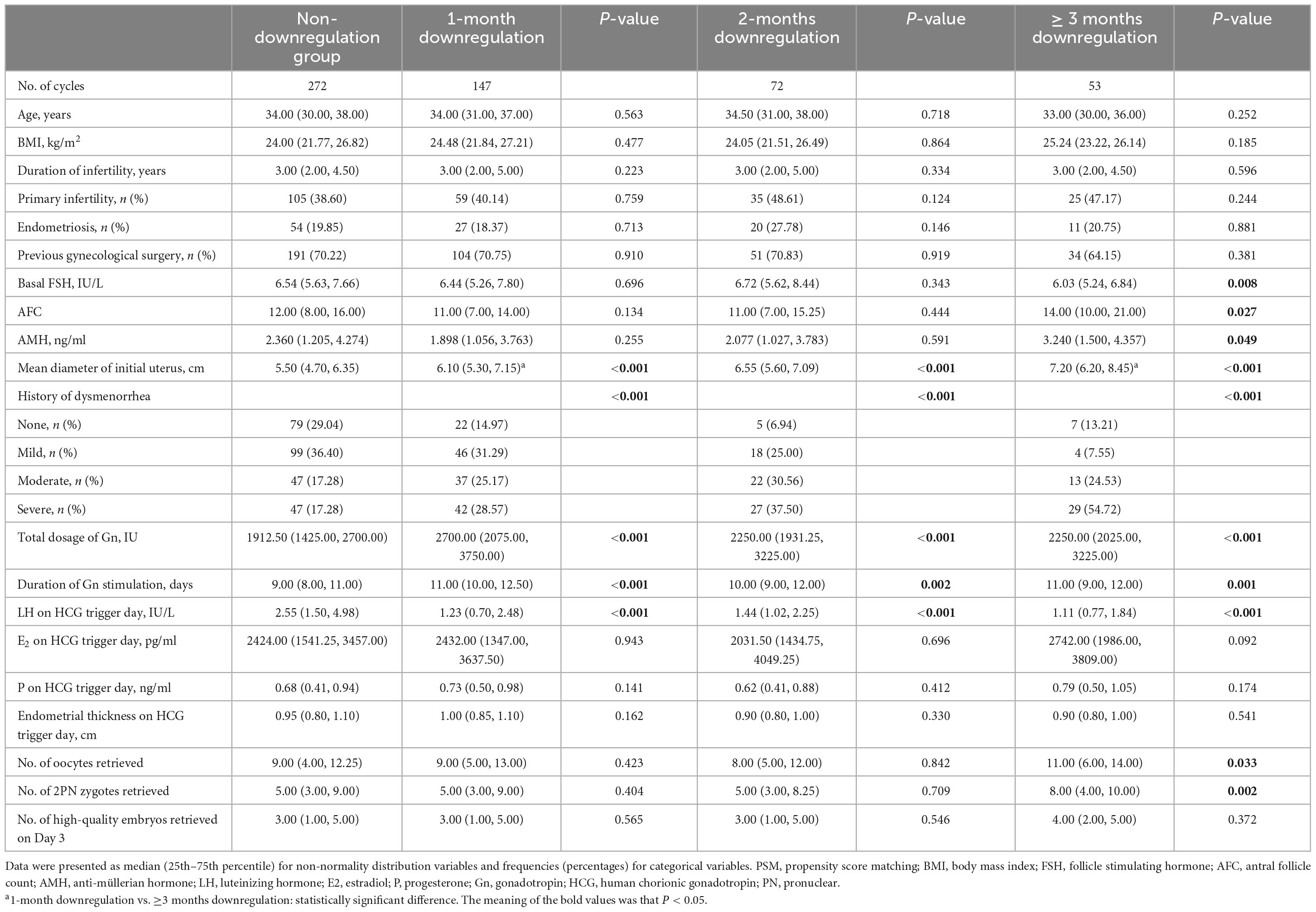
In order to investigate the optimal duration of downregulation, we further divided the matched downregulation group into 1-month downregulation (147 cycles), 2-months downregulation (72 cycles) and ≥3 months downregulation (53 cycles) subgroups according to the duration of long-acting GnRHa downregulation. The characteristics of the study population of each subgroup after PSM were displayed in Table 3. Compared to non-downregulation group, the ≥3 months downregulation group had lower basal FSH (6.03 vs. 6.54 IU/L, P = 0.008), higher AFC (14.00 vs. 12.00, P = 0.027), higher AMH (3.240 vs. 2.360 ng/ml, P = 0.049), more numbers of retrieved oocytes (11.00 vs. 9.00, P = 0.033) and 2PN zygotes (8.00 vs. 5.00, P = 0.002). The proportions of severe dysmenorrhea in the 1-month, 2-months, and ≥3 months downregulation group were respectively 28.57%, 37.50%, and 54.72%, which were obviously higher than the control group (17.28%, P < 0.001). The mean diameter of initial uterus in the 1-month (6.10 vs. 5.50 cm, P < 0.001), 2-months (6.55 vs. 5.50 cm, P < 0.001) and ≥3 months downregulation group (7.20 vs. 5.50 cm, P < 0.001) were significantly larger than the non-downregulation group, and it significantly increased in the ≥3 months downregulation group compared to the 1-month downregulation group. The total dosage of gonadotropin in the 1-month (2700.00 vs. 1912.50, P < 0.001), 2-months (2250.00 vs. 1912.50, P < 0.001) and ≥3 months downregulation group (2250.00 vs. 1912.50, P < 0.001) was significantly higher than the non-downregulation group. The duration of gonadotropin in the 1-month (11.00 vs. 9.00, P < 0.001), 2-months (10.00 vs. 9.00, P = 0.002), and ≥3 months downregulation group (11.00 vs. 9.00, P = 0.001) was significantly longer than the non-downregulation group. Likewise, the LH on HCG trigger day in the 1-month (1.23 vs. 2.55, P < 0.001), 2-months (1.44 vs. 2.55, P < 0.001) and ≥3 months downregulation group (1.11 vs. 2.55, P < 0.001) was significantly lower than the non-downregulation group, respectively. No statistical differences were detected in other parameters between downregulation subgroup and the non-downregulation group.
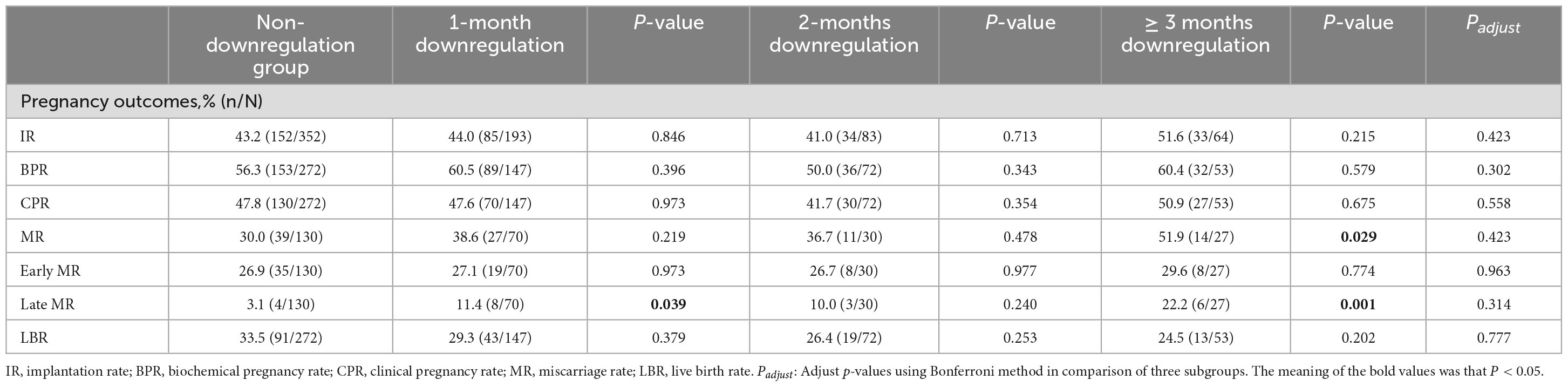
The comparisons of pregnancy outcomes among subgroups were shown in Table 4. There were no significant differences in IR, BPR, CPR, early MR, and LBR in the 1-month, 2-months, and ≥3 months downregulation group compared to the non-downregulation group. However, late MR (11.4% vs. 3.1%, P = 0.039) in the 1-month downregulation group significantly increased compared to the non-downregulation group. MR (51.9% vs. 30.0%, P = 0.029), especially late MR (22.2% vs. 3.1%, P = 0.001) in the ≥3 months downregulation group significantly increased compared to the non-downregulation group. No differences in pregnancy-related parameters were detected in comparisons of downregulation subgroups.
The comparison of pregnancy outcomes stratified by fresh ET or FET cycles were shown in Table 5. A total of 239 fresh ET cycles and 305 FET cycles were included in the stratification analysis. In fresh ET cycles, IR (75.0% vs. 39.2%, P = 0.002), BPR (91.7% vs. 56.0%, P = 0.036), CPR (83.3% vs. 47.0%, P = 0.016) and late MR (30.0% vs. 3.2%, P = 0.017) in the ≥3 months downregulation group significantly increased compared to the non-downregulation group, while no differences were found in MR, early MR and LBR. In intra-subgroup analysis, IR (75.0% vs. 45.5%, P = 0.046) in the ≥3 months downregulation group significantly increased compared to the 1-month downregulation group. In FET cycles, MR (53.6% vs. 29.9%, P = 0.029; 58.8% vs. 29.9%, P = 0.026) significantly increased and LBR (18.8% vs. 34.1%, P = 0.023; 17.1% vs. 34.1%, P = 0.037) significantly decreased in the 1-month and ≥3 months downregulation group compared to the non-downregulation group. However, no differences in pregnancy outcomes were found in the 2-months downregulation group compared to the non-downregulation group.
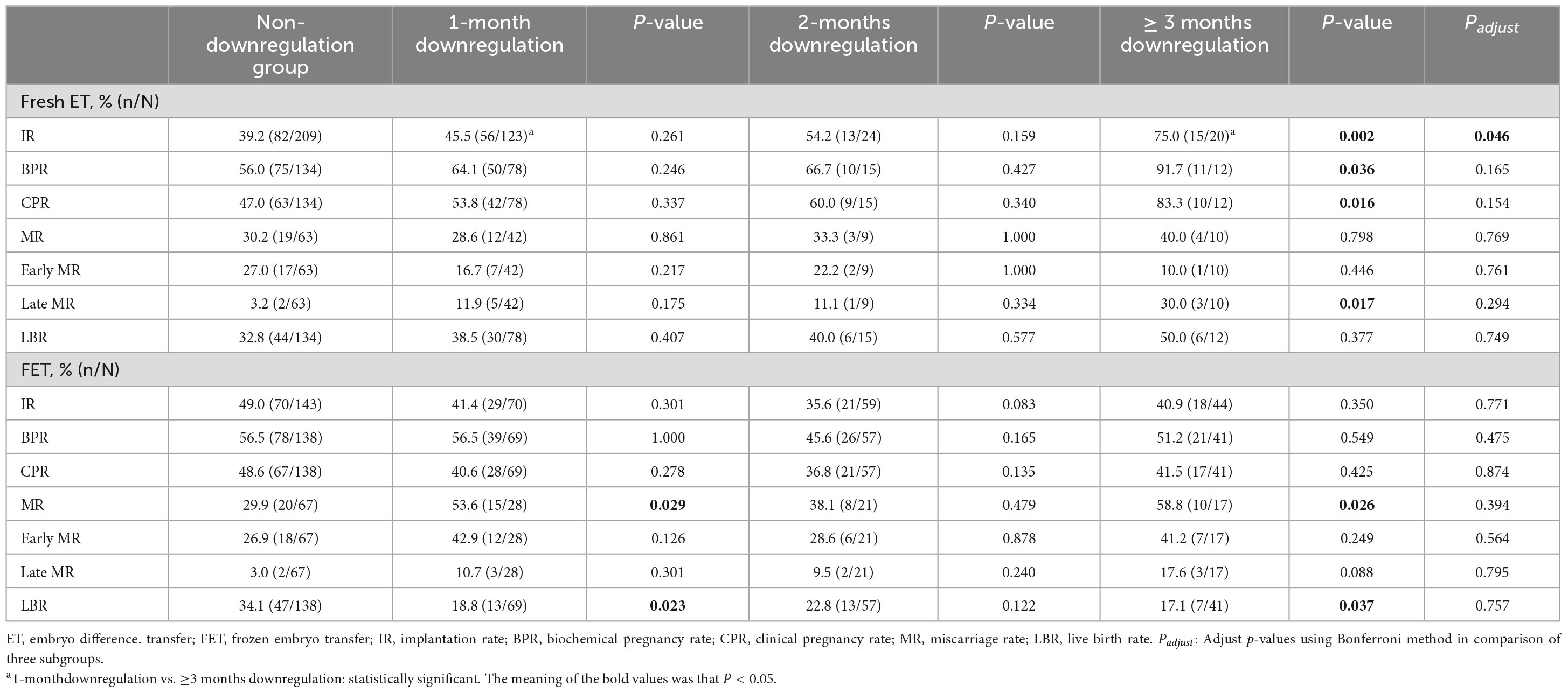
Table 5. Comparison of pregnancy outcomes stratified by fresh ET or FET cycles and subgroup analyses.
Discussion
In our study, an important demographic characteristic was that symptoms of adenomyosis in the downregulation subgroups were severer than those in the non-downregulation group. For adenomyosis patients with severer disease status, long-acting GnRHa downregulation during ART treatment might be related to improved pregnancy outcomes, which needed to be further verified by larger sample studies. In fresh ET cycles, prolonged downregulation (≥3 months) could significantly improve IR, BPR and CPR, while late MR was not synchronously improved. In FET cycles, the optimal duration of downregulation still needs further exploration.
Adenomyosis is a complex disease with eight classical imaging characteristics. Previous studies reported that the number of sonographic features of adenomyosis might be a prognostic indicator of the severe extent of adenomyosis. Patients with more sonographic features were inclined to have larger uterus and severer symptoms, which were intimated with adverse pregnancy outcomes (33–36). In our study, larger mean diameter of initial uterus and higher proportion of severe dysmenorrhea were observed in the downregulation group. However, IR, BPR, CPR, MR, early MR, and LBR were similar between the downregulation group and non-downregulation group, which suggested that long-acting GnRHa downregulation during ART treatment might be related to improved pregnancy outcomes in patients with severer adenomyosis. Additionally, a recent meta-analysis concluded similar conclusions, that was, patients with adenomyosis receiving short GnRHa downregulation protocol were related to significantly decreased CPR and increased MR, whereas the similar correlation was not found in ultra-long GnRHa protocol (37).
In fresh ET cycles, we noticed that IR, BPR, CPR and MR in the 1-month and 2-months downregulation groups were similar to those in the non-downregulation group. After prolonging downregulation (≥3 months), IR, BPR and CPR significantly improved compared to the non-downregulation group, which suggested that for patients with severer adenomyosis, prolonged duration of long-acting GnRHa downregulation prior to COS had advantageous impacts on pregnancy outcomes. The improvement of pregnancy outcomes might be associated with the potential effects of GnRHa, such as increased pulsatility index of uterine arteries, improved endometrial blood flow and ameliorated the endometrial receptivity (23, 38, 39). Besides these, Guo et al. (40) elucidated that GnRHa could significantly increase the expression levels of Hoxa10, Hoxa11, Lif, integrin b3 protein and pinopodes during the implantation window, which improved the endometrial receptivity and pregnancy outcomes in mouse model. Apart from pregnancy-related parameters, we also noticed that numbers of obtained oocytes and 2PN zygotes in the ≥3 months downregulation group were significantly higher than the non-downregulation group. Although long-acting downregulation might result in deeper inhibition of ovary, prolonged duration of gonadotropin and increased total dosage of gonadotropin might promote the growth of slow-growing follicles and make follicles synchronous development, which was beneficial to the increase of retrieved oocytes and improvement of the quality of oocytes and embryos. Different from the FET cycles, the COS in fresh ET cycles could cause obvious hyperestrogenic status to a certain extent, which could promote the enlargement of uterus and offset partial effect of previous long-acting GnRHa downregulation. Consequently, the selection of long-acting GnRHa downregulation and its duration should be considered according to the patient’s comprehensive situation, and our findings required further verification.
In FET cycles, for patients with severer adenomyosis, IR, BPR, CPR, early MR and late MR in the downregulation subgroups had no statistical differences with the non-downregulation group. Compared to the non-downregulation group, MR increased and LBR decreased significantly in the 1-month downregulation group, while no differences were observed in the 2-months downregulation group. The optimal duration of downregulation still needs further exploration. Li et al. (24) reported that the uterine volume reduced to below 98.81 cm3 before FET could significantly decrease MR and increase LBR in patients with adenomyosis. Additionally, Zhang et al. (41) also proposed that in adenomyosis patients with uterine volume between 56 and 100 cm3, better pregnancy outcomes with lower MR and higher LBR could be achieved after long-acting GnRHa downregulation in FET cycles. However, MR in the ≥3 months downregulation group was higher than the non-downregulation group, which might be associated with severer adenomyosis. The increased MR might be associated with defect process of spiral arteries remodeling in the uterine junctional zone and subsequent deep placentation impairment (42, 43). Epithelial-mesenchymal transition (EMT) and fibroblast-to-myofibroblast transdifferentiation (FMT) also played important roles on the continuing development of adenomyosis, which could deteriorate fibrosis of adenomyotic lesions and subsequently weaken the effect of long-acting GnRHa (44, 45). These might be important reasons of negative obstetrical outcomes in patients with adenomyosis, such as increased pregnancy loss and preterm birth, while more detailed mechanisms still needed to be elucidated (46–49). Therefore, long-acting GnRHa downregulation did have positive effects on severer adenomyosis in FET cycles, but the duration of GnRHa still needed further exploration. The factors affecting MR were complex and the effects of GnRHa will gradually vanish with the extension of pregnancy. The detailed mechanism of the correlation between higher MR and adenomyosis needs to be constantly explored.
There were three prominent strengths in our study. Firstly, we adopted PSM approach to eliminate the influence of confounding factors and enhance the comparability between the downregulation group and non-downregulation group. Secondly, subgroup analysis was performed to evaluate the dose-response relationship between the duration of long-acting GnRHa downregulation and pregnancy outcomes. Thirdly, stratification analysis was used to evaluate the different downregulation strategies in fresh ET and FET cycles. Certainly, there were several limitations. The study was single-center, retrospective, and the sample size was limited. The severity of adenomyosis could not be accurately assessed by uterine volume. Therefore, multi-center randomized controlled trials need to be carried out.
Conclusion
In patients with severer adenomyosis, long-acting GnRHa downregulation might be correlated with improved ART outcomes, which needs to be further investigated by larger sample studies. In fresh ET cycles, prolonged downregulation (≥3 months) might improve live birth. In FET cycles, the optimal duration of downregulation still needs further exploration. Our findings provide some reference for clinicians to make individualized fresh ET and FET protocols for adenomyosis patients with different disease status. The mechanism of the correlation between higher MR and adenomyosis needs constant exploration. Randomized controlled trials with larger samples should be designed to verify our findings in the future.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee at the Center for Reproductive Medicine, Shandong University (No. 2021-133). Written informed consent was not required because this is a retrospective study.
Author contributions
LC designed the study and applied for data. YL and XY collected and analyzed the data. YL and LG drafted the manuscript. LG, LC and Z-JC critically reviewed the manuscript. All authors contributed to the manuscript and approved the submitted version.
Funding
This study was funded by The National Key Technology Research and Developmental Program of China (2022YFC2704404), Research Unit of Gametogenesis and Health of ART-Offspring, Chinese Academy of Medical Sciences (2020RU001), China Health Promotion Foundation (Association between ovarian response and embryo quality in women with normal ovarian reserve undergoing in vitro fertilization using a standard long protocol: a retrospective cohort study; Association between the numbers of retrieved oocytes and pregnancy outcomes in women with normal ovarian reserve undergoing in vitro fertilization: a retrospective cohort study), Taishan Scholars Program for Young Experts of Shandong Province (tsqn201909195), and Natural Science Foundation of Shandong Province (ZR2021MH390).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Gordts S, Grimbizis G, Campo R. Symptoms and classification of uterine adenomyosis, including the place of hysteroscopy in diagnosis. Fertil Steril. (2018) 109:380–8.e1. doi: 10.1016/j.fertnstert.2018.01.006
3. Bird CC, McElin TW, Manalo-Estrella P. The elusive adenomyosis of the uterus—revisited. Am J Obstet Gynecol. (1972) 112:583–93.
4. Chapron C, Vannuccini S, Santulli P, Abrão MS, Carmona F, Fraser IS, et al. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum Reprod Update. (2020) 26:392–411. doi: 10.1093/humupd/dmz049
5. Puente JM, Fabris A, Patel J, Patel A, Cerrillo M, Requena A, et al. Adenomyosis in infertile women: prevalence and the role of 3D ultrasound as a marker of severity of the disease. Reprod Biol Endocrinol. (2016) 14:60. doi: 10.1186/s12958-016-0185-6
6. Younes G, Tulandi T. Effects of adenomyosis on in vitro fertilization treatment outcomes: a meta-analysis. Fertil Steril. (2017) 108:483.e–90.e.
7. Buggio L, Dridi D, Barbara G. Adenomyosis: impact on fertility and obstetric outcomes. Reprod Sci. (2021) 28:3081–4.
8. Vigano P, Corti L, Berlanda N. Beyond infertility: obstetrical and postpartum complications associated with endometriosis and adenomyosis. Fertil Steril. (2015) 104:802–12. doi: 10.1016/j.fertnstert.2015.08.030
9. Horton J, Sterrenburg M, Lane S, Maheshwari A, Li TC, Cheong Y. Reproductive, obstetric, and perinatal outcomes of women with adenomyosis and endometriosis: a systematic review and meta-analysis. Hum Reprod Update. (2019) 25:592–632. doi: 10.1093/humupd/dmz012
10. Kissler S, Hamscho N, Zangos S, Wiegratz I, Schlichter S, Menzel C, et al. Uterotubal transport disorder in adenomyosis and endometriosis–a cause for infertility. Int J Obstet Gynaecol. (2006) 113:902–8. doi: 10.1111/j.1471-0528.2006.00970.x
11. Guo S, Zhang D, Lu X, Zhang Q, Gu R, Sun B, et al. Hypoxia and its possible relationship with endometrial receptivity in adenomyosis: a preliminary study. Reprod Biol Endocrinol. (2021) 19:7. doi: 10.1186/s12958-020-00692-y
12. Tanos V, Lingwood L, Balami S. The importance of the junctional zone of the endometrium in human reproduction. Hum Fertil. (2020) 25:4–12.
13. Wu H-M, Chang H-M, Leung PCK. Gonadotropin-releasing hormone analogs: mechanisms of action and clinical applications in female reproduction. Front Neuroendocrinol. (2021) 60:100876.
14. Khan KN, Kitajima M, Hiraki K, Fujishita A, Sekine I, Ishimaru T, et al. Changes in tissue inflammation, angiogenesis and apoptosis in endometriosis, adenomyosis and uterine myoma after GnRH agonist therapy. Hum Reprod. (2010) 25:642–53. doi: 10.1093/humrep/dep437
15. Khan KN, Kitajima M, Hiraki K, Fujishita A, Nakashima M, Ishimaru T, et al. Cell proliferation effect of GnRH agonist on pathological lesions of women with endometriosis, adenomyosis and uterine myoma. Hum Reprod. (2010) 25:2878–90. doi: 10.1093/humrep/deq240
16. Hou X, Xing J, Shan H, Mei J, Sun Y, Yan G, et al. The effect of adenomyosis on IVF after long or ultra-long GnRH agonist treatment. Reprod Biomed Online. (2020) 41:845–53.
17. Sheng Y, Ma C, Yang R, Liu Z, Liu P, Qiao J. Effects of different controlled ovarian hyperstimulation for adenomyosis on the outcomes of IVF-ET. Reproduction and Contraception. (2010) 30:375–8.
18. Lan J, Wu Y, Wu Z, Wu Y, Yang R, Liu Y, et al. Ultra-long GnRH agonist protocol during IVF/ICSI improves pregnancy outcomes in women with adenomyosis: a retrospective cohort study. Front Endocrinol. (2021) 12:609771. doi: 10.3389/fendo.2021.609771
19. Niu Z, Chen Q, Sun Y, Feng Y. Long-term pituitary downregulation before frozen embryo transfer could improve pregnancy outcomes in women with adenomyosis. Gynecol Endocrinol. (2013) 29:1026–30. doi: 10.3109/09513590.2013.824960
20. Guo S, Zhang D, Niu Z, Sun Y, Feng Y. Pregnancy outcomes and neonatal outcomes after pituitary down-regulation in patients with adenomyosis receiving IVF/ICSI and FET: results of a retrospective cohort study. Int J Clin Exp Med. (2016) 9:14313–20.
21. Li M, Xu L, Zhao H, Du Y, Yan L. Effects of artificial cycles with and without gonadotropin-releasing hormone agonist pretreatment on frozen embryo transfer outcomes in patients with adenomyosis. Sci Rep. (2021) 11:19326. doi: 10.1038/s41598-021-98918-5
22. Matsushima T, Akira S, Fukami T, Yoneyama K, Takeshita T. Efficacy of hormonal therapies for decreasing uterine volume in patients with adenomyosis. Gynecol Minim Invasive Ther. (2018) 7:119–23.
23. Xie M, Yu H, Zhang X, Wang W, Ren Y. Elasticity of adenomyosis is increased after GnRHa therapy and is associated with spontaneous pregnancy in infertile patents. J Gynecol Obstet Hum Reprod. (2019) 48:849–53. doi: 10.1016/j.jogoh.2019.05.003
24. Li X, Pan N, Zhang W, Wang Y, Ge Y, Wei H, et al. Association between uterine volume and pregnancy outcomes in adenomyosis patients undergoing frozen-thawed embryo transfer. Reprod Biomed Online. (2021) 42:384–9.
25. Van den Bosch T, Dueholm M, Leone FP, Valentin L, Rasmussen CK, Votino A, et al. Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: a consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet Gynecol. (2015) 46:284–98. doi: 10.1002/uog.14806
26. Bazot M, Daraï E. Role of transvaginal sonography and magnetic resonance imaging in the diagnosis of uterine adenomyosis. Fertil Steril. (2018) 109:389–97.
27. Puissant F, Van Rysselberge M, Barlow P, Deweze J, Leroy F. Embryo scoring as a prognostic tool in IVF treatment. Hum Reprod. (1987) 2:705–8.
28. Xu L, Ding L, Jiang J, Liu P, Wei D, Qin Y. Effects of oral contraceptive pretreatment on IVF outcomes in women following a GnRH agonist protocol. Reprod Biomed Online. (2019) 39:924–30.
29. Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X, Cao Y, et al. Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. N Engl J Med. (2016) 375:523–33.
30. Man Y, Bian Y, Zhao S, Zhao R, Xu X, Wei D, et al. The effect of different endometrial preparations on women with polycystic ovary syndrome undergoing initial frozen embryo transfer: a historical cohort analysis. Acta Obstet Gynecol Scand. (2021) 100:1116–23. doi: 10.1111/aogs.14058
31. Andersch B, Milsom I. An epidemiologic study of young women with dysmenorrhea. Am J Obstet Gynecol. (1982) 144:655–60.
32. Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The international glossary on infertility and fertility care, 2017†‡§. Hum Reprod. (2017) 32:1786–801.
33. Exacoustos C, Morosetti G, Conway F, Camilli S, Martire FG, Lazzeri L, et al. New sonographic classification of adenomyosis: do type and degree of adenomyosis correlate to severity of symptoms? J Minim Invasive Gynecol. (2020) 27:1308–15. doi: 10.1016/j.jmig.2019.09.788
34. Naftalin J, Hoo W, Nunes N, Holland T, Mavrelos D, Jurkovic D. Association between ultrasound features of adenomyosis and severity of menstrual pain. Ultrasound Obstet Gynecol. (2016) 47:779–83.
35. Nishida M. Relationship between the onset of dysmenorrhea and histologic findings in adenomyosis. Am J Obstet Gynecol. (1991) 165:229–31. doi: 10.1016/0002-9378(91)90257-r
36. Pinzauti S, Lazzeri L, Tosti C, Centini G, Orlandini C, Luisi S, et al. Transvaginal sonographic features of diffuse adenomyosis in 18-30-year-old nulligravid women without endometriosis: association with symptoms. Ultrasound Obstet Gynecol. (2015) 46:730–6. doi: 10.1002/uog.14834
37. Nirgianakis K, Kalaitzopoulos DR, Schwartz ASK, Spaanderman M, Kramer BW, Mueller MD, et al. Fertility, pregnancy and neonatal outcomes of patients with adenomyosis: a systematic review and meta-analysis. Reprod Biomed Online. (2021) 42:185–206.
38. Manetta LA, de Paula Martins W, Rosa e Silva JC, de Sa Rosa e Silva AC, Nogueira AA, Ferriani RA. Uterine ultrasonographic changes during endometriosis treatment: a comparison between levonorgestrel-releasing intrauterine devices and a gonadotropin-releasing hormone agonist. Ultrasound Med Biol. (2008) 34:1914–8. doi: 10.1016/j.ultrasmedbio.2008.04.013
39. Chien LW, Au HK, Chen PL, Xiao J, Tzeng CR. Assessment of uterine receptivity by the endometrial-subendometrial blood flow distribution pattern in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. (2002) 78:245–51. doi: 10.1016/s0015-0282(02)03223-5
40. Guo S, Li Z, Yan L, Sun Y, Feng Y. GnRH agonist improves pregnancy outcome in mice with induced adenomyosis by restoring endometrial receptivity. Drug Des Dev Ther. (2018) 12:1621–31. doi: 10.2147/DDDT.S162541
41. Zhang W, Han B, Ma C, Qiao J. Effect of GnRH-a pretreatment before frozen-thawed embryo transfer on pregnancy outcome of adenomyosis-associated infertile patients with 56 cm3 ≤ uterine volume ≤ 100 cm3. Ann Transl Med. (2022) 10:509. doi: 10.21037/atm-21-6247
42. Brosens I, Pijnenborg R, Vercruysse L, Romero R. The “great obstetrical syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol. (2011) 204:193–201.
43. Brosens I, Pijnenborg R, Benagiano G. Defective myometrial spiral artery remodelling as a cause of major obstetrical syndromes in endometriosis and adenomyosis. Placenta. (2013) 34:100–5. doi: 10.1016/j.placenta.2012.11.017
44. Liu X, Shen M, Qi Q, Zhang H, Guo SW. Corroborating evidence for platelet-induced epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation in the development of adenomyosis. Hum Reprod. (2016) 31:734–49.
45. Shen M, Liu X, Zhang H, Guo SW. Transforming growth factor β1 signaling coincides with epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation in the development of adenomyosis in mice. Hum Reprod. (2016) 31:355–69.
46. Atabekoğlu CS, Şükür YE, Kalafat E, Özmen B, Berker B, Aytaç R, et al. The association between adenomyosis and recurrent miscarriage. Eur J Obstet Gynecol Reprod Biol. (2020) 250:107–11.
47. Martínez-Conejero JA, Morgan M, Montesinos M, Fortuño S, Meseguer M, Simón C, et al. Adenomyosis does not affect implantation, but is associated with miscarriage in patients undergoing oocyte donation. Fertil Steril. (2011) 96:943–50.
48. Stanekova V, Woodman RJ, Tremellen K. The rate of euploid miscarriage is increased in the setting of adenomyosis. Hum Reprod Open. (2018) 2018:hoy011.
Keywords: adenomyosis, GnRH agonist, downregulation, pregnancy outcome, assisted reproductive technology
Citation: Li Y, Ge L, Yang X, Cui L and Chen Z-J (2023) Effects of duration of long-acting GnRH agonist downregulation on assisted reproductive technology outcomes in patients with adenomyosis: a retrospective cohort study. Front. Med. 10:1248274. doi: 10.3389/fmed.2023.1248274
Received: 27 June 2023; Accepted: 12 September 2023;
Published: 26 September 2023.
Edited by:
Simcha Yagel, Hadassah Medical Center, IsraelReviewed by:
Bhuchitra Singh, Johns Hopkins University, United StatesChenyang Huang, Nanjing Drum Tower Hospital, China
Copyright © 2023 Li, Ge, Yang, Cui and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linlin Cui, fdclear3@126.com
†These authors have contributed equally to this work
 Yexing Li1,2,3,4,5,6,7†
Yexing Li1,2,3,4,5,6,7†  Linlin Cui
Linlin Cui